Why in the News?
In the 79th United Nations General Assembly (UNGA) High-Level Meeting on Antimicrobial Resistance (AMR), Global leaders have approved a political declaration on antimicrobial resistance (AMR).
More on the News
- The declaration establishes clear actions and targets aimed at reducing the estimated 4.95 million annual human deaths linked to bacterial AMR by 10% by 2030.
- Declaration also calls for sustainable national funding and an additional US$100 million in catalytic funding to combat AMR.
- Declaration called for following:
- Global multisectoral action that needed to reach targets by 2030.
- On human health: at least 70% of antibiotics used for human health globally should belong to the WHO Access group antibiotics.
- On agriculture and animal health: meaningfully reduce the quantity of antimicrobials used globally in the agri-food systems by 2030.
- On the environment: declaration underscores the need to prevent and address the discharge of antimicrobials into the environment.
What is Anti-Microbial Resistance (AMR)?
- AMR is a condition when microorganisms such as bacteria, viruses, fungi, and parasites change in ways that render the medications used to cure the infections they cause ineffective.
- Major factors contributing to AMR:
- Pharmaceutical Manufacturing: Industrial waste from production of Active Pharmaceutical Ingredients (APIs) for antibiotics.
- Agriculture: Overuse of antibiotics for growth in sectors like livestock, aquaculture, etc.
- Healthcare Facilities: Improper management of unused medications, patient excretion, and disposal of expired drugs.
- Waste Management: Landfill leachate, untreated wastewater, and sewage effluents.
Why AMR is a Global Health threat?
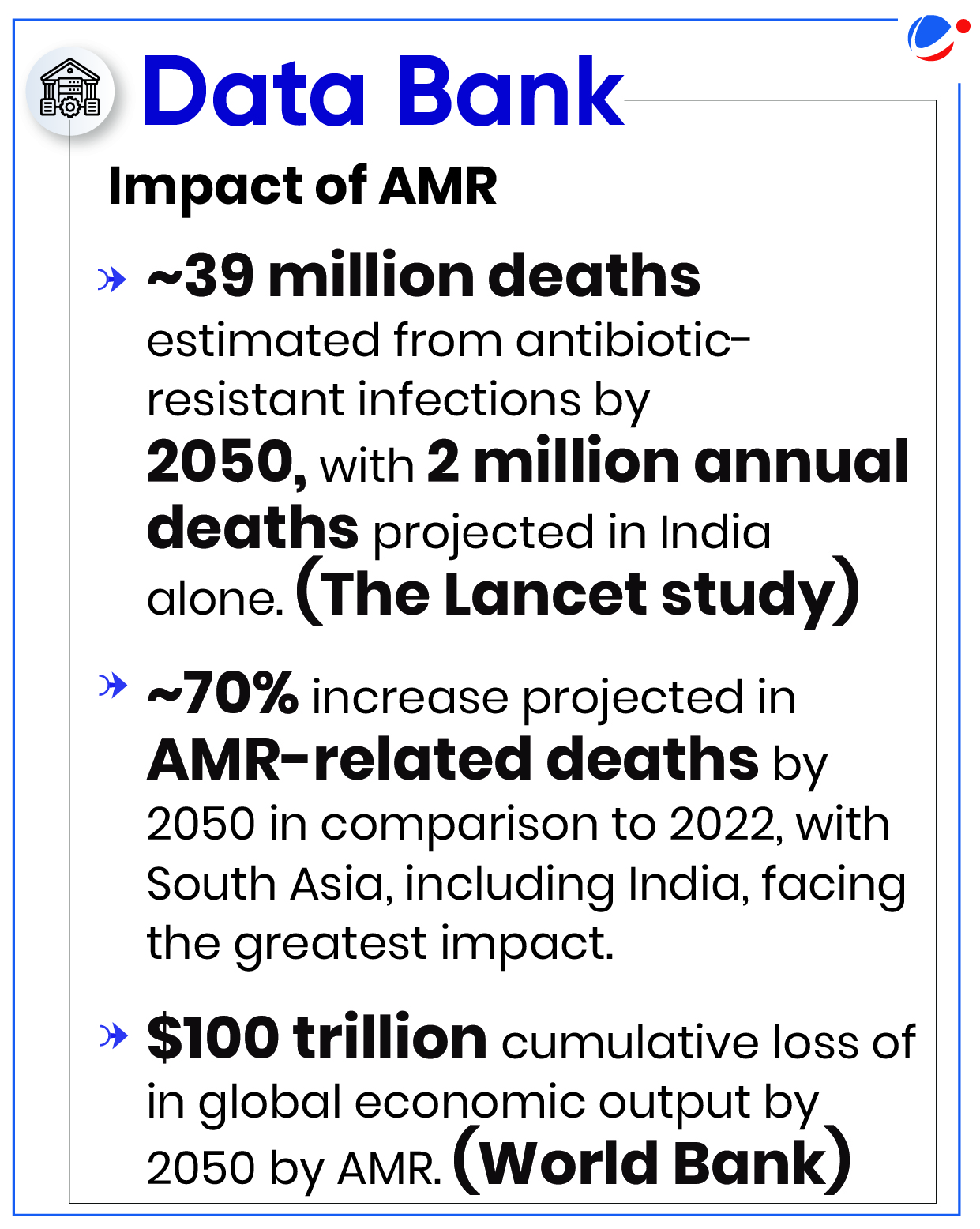
- Economic cost: The World Bank estimates that AMR could result in US$ 1 trillion additional healthcare costs by 2050.
- Drug-resistant infections also impact the health of animals and plants, reduce productivity in farms, and threaten food security.
- Gains of modern medicine at risk: It makes infections harder to treat and makes other medical procedures and treatments – such as surgery, caesarean sections and cancer chemotherapy – much riskier.
- Widespread environmental contamination: Improper disposal of antibiotics leads to environmental contamination, creating reservoirs for resistance genes.
- Impact on Vulnerable Populations: Individuals with weakened immune systems, the elderly, and children are particularly vulnerable to AMR-related infections.
- Limited R&D for alternatives: There is an inadequate research and development pipeline for alternative treatments in the face of rising levels of resistance.
Way Forward
- Implementing WHO Guidance on Wastewater and Solid Waste Management for Antibiotic Manufacturing: It sets targets for liquid effluent, solid waste and Zero Liquid Discharge (ZLD) from pharmaceutical manufacturing. It also makes following recommendations such as–
- Use established tools like hazard analysis etc., along with internal audits and public communication.
- Conduct external audit and certification to ensure robust implementation of risk management plans and to verify performance against targets.
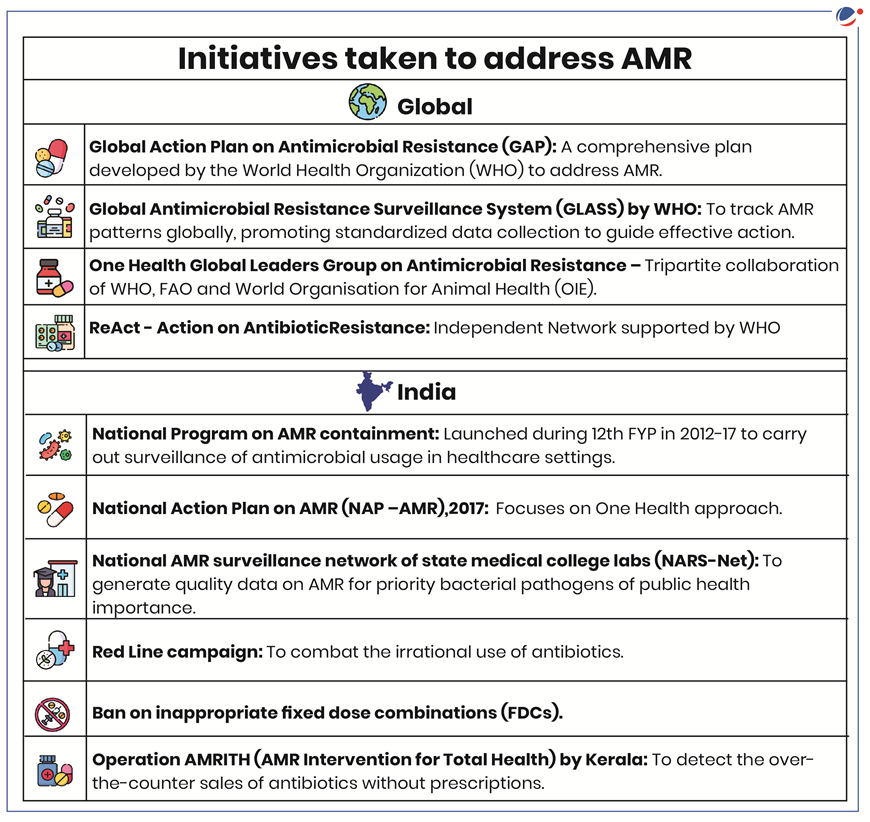
- One Health Approach: Recognize the interconnectedness of human, animal, and environmental health and address AMR in a holistic manner.
- Strengthening Regulations: Environment (Protection) Amendment Rules, 2019, which impose stringent limits on residues of 121 antibiotics in treated effluents from drug production units, should be effectively implemented.
- Agriculture Operations: Sustainable farming practices such as organic farming can be promoted to limit the use of antibiotics in livestock and aquaculture.
- Promoting Responsible Use: Healthcare facilities should implement antibiotic stewardship programs for responsible antibiotic use.
Related NewsAntibiotics in the definition of New Drugs
|