Why in the news?
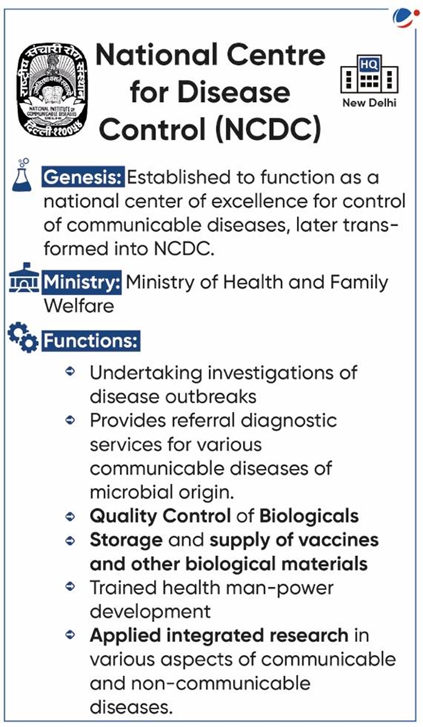
The First Multicentric Point Prevalence Survey of Antibiotic Use was released recently by the National Centre for Disease Control under the Union Health Ministry.
About the survey
- The survey has mapped the patients treated across 15 States and two Union Territories between November 2021 and April 2022.
- Key Findings:
- Empirical prescriptions: 94% of patients surveyed were given antibiotics before medical diagnosis of cause of infection.
- Preventive usage: 55% of patients were prescribed antibiotics for preventive indications, while 45% for therapeutic indications.
- High prevalence of antibiotic usage: At 71.9%.
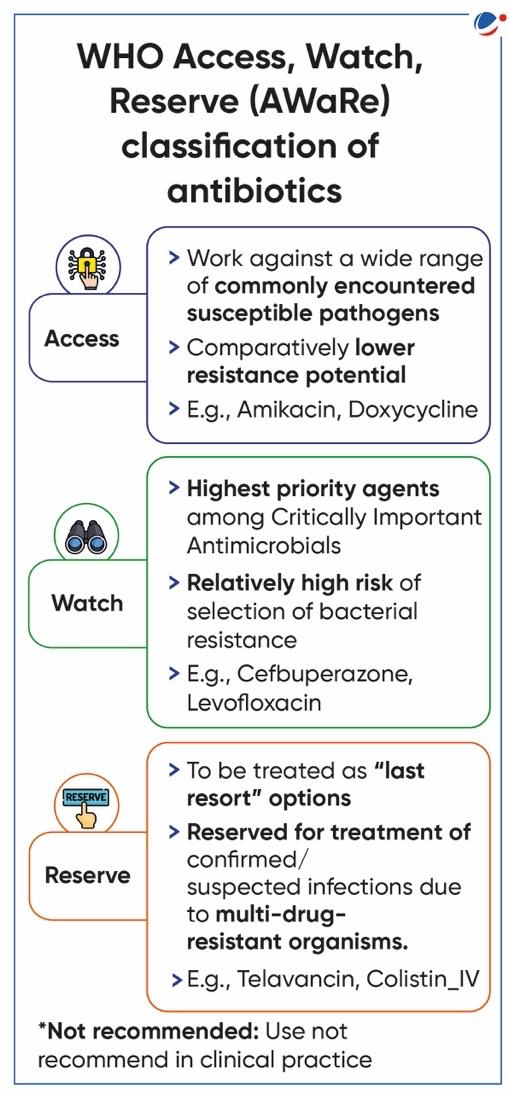
- Classification of prescriptions based on AWaRe groups: 57% from watch groups, 38% from access group and 2% from reserve group.
- 3% of the prescription from not recommended group.
- Only 8 out of 20 institutes surveyed have an antibiotic policy in place.
- The high use of watch group antibiotics raises concern as these antibiotics have a higher potential to develop antibiotic resistance.
About Antimicrobial resistance (AMR)
- AMR happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them.
- While some microorganisms are naturally resistant to a certain type of antimicrobials, they can also acquire resistance genes, whether by spontaneous mutation or through genetic exchange.
- Reasons behind increasing incidence of Antimicrobial resistance
- Overuse and misuse of antimicrobials among humans and in poultry and farm animals.
- Poor infection prevention and control practices in healthcare settings
- Effluents discharge from hospitals, industries, and urban settlements
- Over 75% of administered antibiotics are excreted unmetabolized in urine and faeces and enter into sewage systems and water bodies.
- Confusion over treatment guidelines.
- E.g., the optimal duration of antibiotic therapy for common infections like pneumonia was not established for decades.
Implications of the Spread of Antimicrobial Resistance
- Healthcare Impact: Increased mortality and morbidity, and prolonged illness because infections caused by resistant microorganisms are often more difficult to treat.
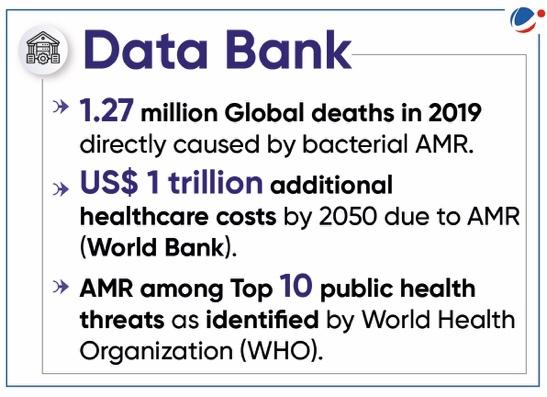
- Increased Healthcare Costs: Longer hospital stays, additional diagnostic tests, and more expensive second-line or third-line antibiotics leads to increased expenditure.
- Economic impact: Working hours lost due to prolonged illness and increase in out-of-pocket expenditure.
- If not controlled, antimicrobial resistance will result in US$ 1 trillion to 3.4 trillion annual losses to gross domestic product (GDP) by 2030. (World Bank)
- Increased risk of outbreaks: As current medicines become ineffective, infections persist in the body, increasing the risk of spreading to others.
- Limited new options for treatment: There are limited new antibiotics in the research and development pipeline.
Measures taken to address AMRNational
Global
|
Way forward
- Promote the judicious use of drugs: For instance, Union Health Ministry has called on doctors in medical colleges and medical associations to make it mandatory to mention the indication and reason for prescribing antibiotics.
- Strict implementations of Drugs and Cosmetics Rules, 1945: Recently, the Director General of Health Services (DGHS) has urged all pharmacist associations to adhere to the rules and sell antibiotics only with valid prescriptions.
- Adherence to standard treatment guidelines and infection control practices: To mitigate antibiotic resistance.
- Defined Antibiotic Use Policy in medical institutes: It should encourage use of access group antibiotics and keep the consumption of reserve group antibiotics at low levels.
- Surveillance and Monitoring of Pathogens: For early detection of resistant strains.
- Robust Immunisation Programmes: The incidence of bacterial and viral infections can be reduced by the adoption of strategies and programmes on the prevention and control of infectious diseases.
- Curbing the Production and Sale of Poor Quality and Sub-standard Antimicrobials: Continuous exposure of bacteria to a sub-therapeutic level of drugs, which is achieved with the use of substandard antimicrobials, always triggers the development of resistance.
- Promote use of alternatives to Antibiotics: In the animal feed industry.
- Educational and Awareness Programme: Strengthen information and resources by involving all stakeholders i.e., policymakers, pharmaceutical industries, medical and veterinary professionals, producers and consumers.